Abstract
Multiple studies have examined the impact of the intensity of conditioning regimens on myeloablation and the risk of relapse after HCT. In contrast to adoptive cell transfer and Chimeric-Antigen Receptor (CAR) T-Cell therapy, there is limited, if any knowledge that has addressed the impact of intensity of lymphodepletion on relapse after HID HCT.
We hypothesize that enhanced lympho-depletion would create an enhanced host immunogenic microenvironment that would foster potent donor T cell expansion and alloreactivity after T-cell replete peripheral blood HID HCT.1,2 We utilized an intensified lympho-depleting conditioning regimen with Fludarabine (Flu) 150 mg/m2, Melphalan (Mel) 140 mg/m2 and Cyclophosphamide (CY) 29 mg/m2 prior to T-cell replete peripheral blood HID HCT to treat 15 consecutive patients with high risk hematological malignancies between July 2015 and June 2017. The intensity of lymphodepletion was confirmed in 12 evaluable patients at day (0) by complete absence of lymphocytes in peripheral smear. In contrast, myeloid elements were detected in 7/12 patients suggesting more intense lympho-depletion than myeloablation.
All Patients received graft versus host disease prophylaxis with Tacrolimus/Mycophenolate starting at day +5 and Cyclophosphamide 50 mg/Kg on day +3 & +4. Mycophenolate continued for 30 days and Tacrolimus stopped at Day 180 without taper.
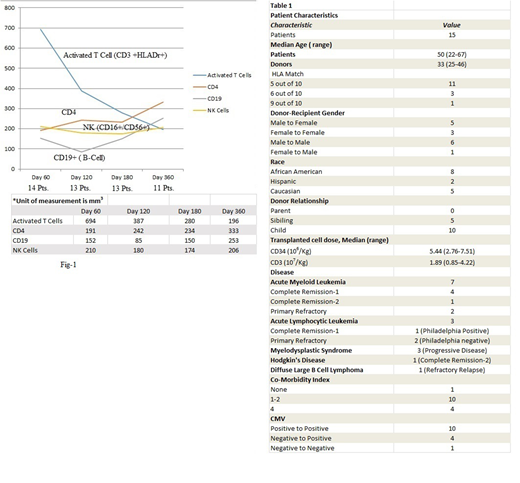
Patient characteristics are shown in Table 1. More than half the patients (n=8 Pts) had relapsed/refractory or progressive disease at time of transplant. The median duration of follow up for survivors is 29 months (range 13-37). Chimerism studies were performed at day +30 and +100 post-transplant by variable number tandem repeat PCR analysis of peripheral blood (PB) and bone marrow (BM). All patients engrafted and achieved 100% Chimerism in BM and PB ( CD3, CD33 & CD56) by day 100 except for 1 patient who died at day +25 prior to engraftment. Median time to neutrophil engraftment was 21 days (range 12-57). All patients with refractory/relapsed disease achieved complete remission post-transplant except for 1 patient who died from transplant complications prior to engraftment. The day 100, 1 year & 2 year overall survival was 93%, 73% & 66% respectively. We observed very low cumulative incidence of relapse of 7% at day 100, 1 and 2 years post-HCT (only 1/15 patients). Treatment related mortality (TRM) was 6%, 20% and 27% at day 100, 1 and 2 years respectively (4/15 patients). Severe Cytokine Release Syndrome (CRS), grade 4 by Lee Criteria occurred in 4 patients, all of them have died at day 25, 258, 288 and 540 post HCT. Three of the four patients with severe CRS had refractory relapsed disease at time of HCT.
Grade II-IV acute GVHD developed in 4/15 patients (27%), 2 of whom had grade III-IV by day +180. Chronic extensive GVHD developed in 7 patients (46%), which required definitive therapy (Prednisone/Rituximab/Extracorporeal Photopheresis). At 2 years post HCT, only 1/7 patients remain with extensive chronic GVHD requiring active treatment, 3 patients have quiescent disease and 3 patients have died. Post -transplant immune reconstitution panels were obtained at day 60, 120, 180 and 1 year in 14, 13, 13 and 10 evaluable patients respectively as shown in Fig 1. We observed early recovery in all T-cell subsets at day 60 with activated T cells (CD3+, HLA-Dr+) being most pronounced. While the early proliferation in activated T cells declined through the first-year post transplant, NK cells and CD4 maintained their early recovery through the first year. There was initial decline in the number of B cells at day 120 which gradually recovered by 1 year.
Conclusion:
Enhanced lymphodepletion prior to peripheral blood HID HCT may enhance early T cell proliferation alloreactivity and immune reconstitution. There was low relapse rate at the expense of high TRM in patients who developed grade IV CRS. Future strategies directed at decreasing disease burden prior to lympho-depletion and improved management of severe CRS in high risk patients are needed to harness the benefits of the observed low relapse rate.
1. Beavis et al, Reprogramming the tumor microenvironment to enhance adoptive cellular therapy. Semin Immunol. 2016 Feb;28(1):64-72.
2. Lu X, Ding ZC, Cao Y, Liu C, Habtetsion T, Yu M, Lemos H, Mellor AL, et al. Alkylating agent melphalan augments the efficacy of adoptive immunotherapy using tumor-specific CD4+ T cells.J Immunol. 2015 Feb 15;194(4):2011-21.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal